
Urinary incontinence during physical exertion: concrete solutions through pelvic floor physiotherapy
Have you ever experienced urinary leakage while running? Although common, they are not normal. This article aims to inform you about urinary incontinence (UI), pelvic anatomy, and your options if, like 62.2% of long-distance runners, you experience leakage. Be aware that this is a broad and complex subject, and we will focus on the main points.
WHAT ARE THE TYPES OF URINARY INCONTINENCE (UI)?
There are several types of UI. The 3 main types are;
- Urgency urinary incontinence (due to overactive bladder);
- Stress urinary incontinence
- Mixed urinary incontinence, a combination of the first two types.
Stress UI and urgency UI are very common among runners. It is a multifactorial condition characterized by the involuntary loss of a small amount of urine. In the case of stress UI, leakage is due to increased intra-abdominal pressure during exercise, coughing, or sneezing. Urgency UI is the sudden onset of a urge to urinate that is so pressing that it is difficult to reach the toilet without leakage.
WHAT ARE THE RISK FACTORS FOR STRESS URINARY INCONTINENCE?
- Gender (predominantly female)
- Age (1 out of 3 of 40 years and over)
- Obesity
- Pregnancy and vaginal delivery
- Multiple pregnancy
- Obstetric trauma (forceps, vacuum, tear)
- Pelvic or gynecological surgery
- Some chronic diseases
- Chronic constipation
- Medication
- Smoking
- Intense physical activity
- Sedentary lifestyle
- Etc.
UNDERSTANDING THE ANATOMY OF THE PELVIS IN RELATION TO THE UI
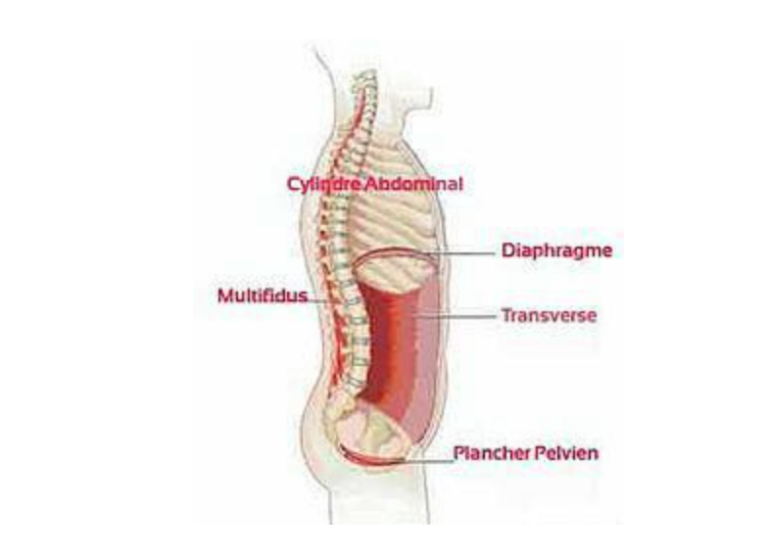
The abdominal cavity is formed by the muscles of the diaphragm (muscle responsible for breathing), the transversus abdominis (the deepest abdominal muscle) and the pelvic floor (structures, muscles, ligaments, nerves, and blood vessels that form the base of the abdominal cavity). Inside this cavity, there is a certain pressure called intra-abdominal pressure (IAP). The IAP changes with breathing, ground impact force, and muscle activation, among other factors.
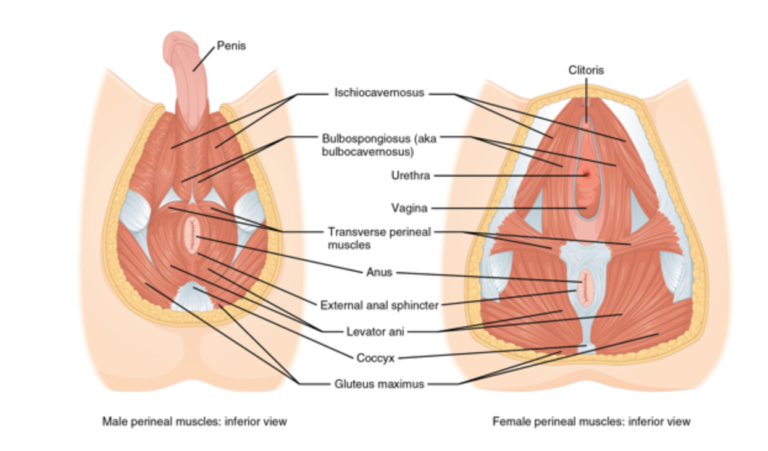
The pelvic floor is made up of 3 layers: superficial, intermediate, and deep. These muscles have several functions:
- Sphincters: control the opening and closing of the urethra, vagina, and rectum.
- Stability: aids in stabilizing the pelvic, back, and hip joints as well as supporting the bladder, uterus, and rectum.
- Pumps: aid in the venous and lymphatic return from the pelvic region.
- Sexual: erection, arousal, and orgasm.
(Hodges 2007, Masters and Johnson 1963, Mitchell 1999, Safik 2011)
https://uresta.com/fr/what-is-the-pelvic-floor-and-what-does-it-do-in-my-body/ (https://uresta.com/fr/what-is-the-pelvic-floor-and-what-does-it-do-in-my-body/)
The pelvic floor is therefore like a group of muscles forming a hammock between the pubic bone, the buttocks (ischial tuberosity), and the sacrum. It supports the organs, and its contraction squeezes the urethra (along with the contraction of the sphincters), thus preventing leakage. It must therefore be able to contract and relax at the right time and at the right speed. In fact, it is not only muscle strength that maintains continence, but also nerve and blood supply. We therefore talk about strength, but also endurance, flexibility, speed, coordination, and synchronization. All of these functions can be assessed in perineal physiotherapy.
Schedule an appointment by clicking here HOW DOES URINARY INCONTINENCE OCCUR DURING RUNNING?During the race, the ground reaction force increases up to 3.9 times the body weight. The IAP also increases with running which requires optimal pelvic health to counter this force and to preserve the mechanisms that allow for continence. However, UI can be caused by several factors. For example:
- Overactivity of the pelvic floor muscles
- A decrease in strength or endurance
- A lack of coordination or speed
- Respiratory issues
- Ineffective strategies for maintaining adequate PIA
- Inadequate ligament support or fascia
- Disorders of nerve conduction or blood supply to these tissues.
An assessment is therefore necessary to determine the causes and guide the treatment.
Several researchers are currently interested in the influence of running patterns on the mechanisms of urinary incontinence. Indeed, a hypothesis has been put forward about the increase in impact force on the pelvic floor depending on the running pattern by comparing heel strike versus forefoot strike. This hypothesis has not yet been proven and further research is needed to confirm or refute this hypothesis. The physiotherapist could, however, suggest different running strategies and evaluate the impact of these changes on your urinary symptoms.
The type of shoe can also have an impact. Indeed, the muscular activity of the pelvic floor muscles is higher when wearing minimalist shoes compared to more maximalist regular shoes.
In men, UI may indicate that the prostate should be examined by a doctor. Indeed, certain conditions such as benign prostatic hyperplasia can lead to signs and symptoms such as leakage. If you have ever had a prostate issue or cancer, or if it has been removed, be aware that physiotherapy can help you regain continence and improve sexual function.
WHAT TYPE OF TREATMENT COULD HELP ME WITH URINARY INCONTINENCE?
Are you familiar with Kegels? In 1940, Dr. Arnold Kegel discovered that it was beneficial for women to strengthen their pelvic floor. These exercises involve contracting the pelvic floor muscles, holding, and then releasing. Since then, these exercises have been overprescribed. However, they are not suitable for everyone! In athletes, the pelvic floor is often hyperactive and has difficulty relaxing, the same goes during pregnancy. Learning how to properly relax your pelvic floor could therefore be more beneficial than strengthening it! Both men and women can benefit from it.
The first thing to do is to make an appointment with a pelvic floor and perineal physiotherapist (https://poglobalite.com/physiotherapie-perineale/). During your meetings, she will be able to assess your pelvic floor, back, hips, abdominals, and anything else that may be relevant in a holistic approach focused on the individual. Indeed, several studies show an association between lower back pain and urinary incontinence (Eliasson, 2008). An internal evaluation (intravaginal or intrarectal) could be performed to properly identify the issue and provide education. Indeed, about 50% of people do not know how to contract their pelvic floor muscles. Furthermore, perineal rehabilitation has been proven very effective for the treatment of UI (evidence level 1 grade A; as a first line of conservative treatment).
If you are consulting in the postpartum period, the assessment will take into account the important aspects for a safe return to running and without symptoms.
Proper tracking will help you increase your body awareness and regain control of your bladder!
REFERENCES
Bo, K., Nygaard, I.E. (2020) Is Physical Activity Good or Bad for the Female Pelvic Floor? A Narrative Review. Sports Med 50, 471-484. https://doi.org/10.1007/s40279-019-01243-1 (https://doi.org/10.1007/s40279-019-01243-1)
Cacciari, L.P., Dumoulin, C., Hay-Smith, J. (2019) Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women: a Cochrane systematic review abridged republication. Brazilian Journal of Physical Therapy, Volume 23, Issue 2, Pages 93-107, ISSN 1413-3555, https://doi.org/10.1016/j.bjpt.2019.01.002 (https://doi.org/10.1016/j.bjpt.2019.01.002).
De Melo Silva, R., Rodrigues, M.E.S., Puga, G.M. et al. (2020). The relationship between running kinematics and the pelvic floor muscle of female runners. International Urogynecology Journal 31, 155-163 https://doi.org/10.1007/s00192-019-04014-8 (https://doi.org/10.1007/s00192-019-04014-8)
Hannestad, Y.S., Rortveit, G., Sandvik, H., Hunskaar, S. (2000) A community-based epidemiological survey of female urinary incontinence: The Norwegian EPINCONT Study, Journal of Clinical Epidemiology, Volume 53, Issue 11, Pages 1150-1157, ISSN 0895-4356, https://doi.org/10.1016/S0895-4356(00)00232-8 (https://doi.org/10.1016/S0895-4356(00)00232-8)
Karmakar, D. and Dwyer, P.L. (2018), High impact exercise may cause pelvic floor dysfunction: FOR: Scale, strengthen, protect! BJOG: Int J Obstet Gy, 125 : 614-614. doi:10.1111/1471-0528.15025 (https://doi.org/10.1111/1471-0528.15025)
Koenig, I., Eichelberg, P., Leitner, M., Moser, H., Kuhn, A., Taeymans, J. and Radlinger, L. (2019) Pelvic floor muscle activity patterns in women with and without stress urinary incontinence while running. [Online] Annals of Physical and Rehabilitation Medicine, https://doi.org/10.1016/j.rehab.2019.09.013 (https://doi-org.proxy.bib.uottawa.ca/10.1016/j.rehab.2019.09.013)
Kruger, J. (2018), High impact exercise may cause pelvic floor dysfunction: AGAINST: Is high‐impact exercise really bad for your pelvic floor? BJOG: Int J Obstet Gy, 125: 615-615. Doi:10.1111/1471-0528.15024 (https://doi.org/10.1111/1471-0528.15024)
Leitner (https://onlinelibrary-wiley-com.proxy.bib.uottawa.ca/action/doSearch?ContribAuthorStored=Leitner%2C+Monika), M., Moser (https://onlinelibrary-wiley-com.proxy.bib.uottawa.ca/action/doSearch?ContribAuthorStored=Moser%2C+Helene), H., Eichelberger (https://onlinelibrary-wiley-com.proxy.bib.uottawa.ca/action/doSearch?ContribAuthorStored=Eichelberger%2C+Patric), P., Kuhn (https://onlinelibrary-wiley-com.proxy.bib.uottawa.ca/action/doSearch?ContribAuthorStored=Kuhn%2C+Annette), A. and Radlinger (https://onlinelibrary-wiley-com.proxy.bib.uottawa.ca/action/doSearch?ContribAuthorStored=Radlinger%2C+Lorenz), L. (2016). Evaluation of pelvic floor muscle activity during running in continent and incontinent women: An exploratory study. Wiley Periodicals, Inc. https://doi-org.proxy.bib.uottawa.ca/10.1002/nau.23151 (https://doi-org.proxy.bib.uottawa.ca/10.1002/nau.23151)
María García-Arrabe, Pablo García-Fernández, Beatriz Ruiz-Ruiz et al. Effects of Minimalist Shoes on Pelvic Floor Activity in Nulliparous Women During Running at Different Velocities: a Randomized Cross-over Clinical Trial, July 22, 2022, PREPRINT (Version 1) available at Research Square [https://doi.org/10.21203/rs.3.rs-1806986/v1 (https://doi.org/10.21203/rs.3.rs-1806986/v1)]

Back pain: how physiotherapy relieves lo...
Persistent lower back pain? Discover how physiotherapy can effectively relieve your backache with a ...
Lire plus...
Mental health and rehabilitation: an und...
Mental health, often overlooked, plays a crucial role in the success of a rehabilitation process. Di...
Lire plus...
Osteopathy and cranial deformities: a ge...
Does your baby have a cranial deformity? Pediatric osteopathy, complementary to physiotherapy, can p...
Lire plus...